The second wave of the C19 Pandemic has completely exposed the severe limitations in India’s healthcare value chain. We all experienced helplessness as we saw the health system collapse in front of our eyes, the brave fight and sacrifices by our doctors and healthcare workers, despite their best efforts we lost precious lives and experienced extreme suffering. It has left many innocents orphaned or disabled, leaving behind scars in the memories of our next generations, that would be difficult to erase. The issue is systemic and chronic, aggravated over time of neglect, and the root causes are not intuitively obvious, which sprouts primarily from two factors, that are fundamental to value creation namely:
To understand the interplay of these two factors, let us look at both the supply side as well as the demand side of this problem first from the macro perspective of policies, structure, and competition, and the potential direction of a solution, that may help salvage India’s broken healthcare system.
The genesis of the traumatic experience lies in the permanent crisis of our public health system, which has arisen due to the cumulative effects of political apathies, shallow policies, and erroneous attempts of reforms to fix the problem rather than solve it, at the wrong places and at the wrong times. These flawed attempts have been consistently pursued by most of the governments in power over the last 74 years, since our Independence. Whether in the state or the center, the power structure has always over-promised in their election manifestos but delivered little on their promises for building the public health infrastructure, particularly in semi-urban and rural areas. They have kept this vital social pillar of our country ‘weak by design’, to further the vote bank objectives based on preserving the dependence within our communities, exercising control, and maintaining ‘bargaining power’ for votes. Healthcare being a state subject, has always resulted in political squabbles between the center and state on the issue of funding and authority, as we are experiencing in the case of C19 vaccines, even under an extreme national crisis depicting the lack of national character.
This weak health pillar of our society has placed constraints on our economic growth, by impacting the quality of our human capital. Adam Smith in his seminal work, ‘Wealth of Nations’, emphasized that a healthy and educated human capital is the secret behind why some nations who nurture it properly, grow wealthy and those who ignore it, languish. Weak health infrastructure has prevented India from leveraging the demographic dividend of youth and harvesting the abundant talents, needed to become a truly global economic power. We are obligated to our children and future generations to correct this, else posterity shall never forgive us.
Most of our leaders’ political will and lack of intent has fallen short by quite a distance for developing a sound public health system. This lack of intent is evident from the fact, that the national allocation for public health is just hovering around 1.5% of GDP, which is one of the lowest in the world. This may be compared to a 10% to 16% GDP range of healthcare spending by leading nations such as the UK, USA, and all major European countries. Even Asian powerhouses like China, South Korea, etc allocates 5 % to 7% of GDP for public healthcare. So it is quite clear that public healthcare has never been considered a priority and is heavily under-resourced, by our political leaders.
Thus the low GDP allocation of 1.5% represents the first nail in our healthcare coffin.
The basic availability of healthcare services in the semi-urban and rural areas is a major issue, where more than 80% of India’s population resides, yet barely 20% of our healthcare force and doctors work in these geographic areas.
The 80:20 availability ratio of the healthcare workforce represents the second nail in our healthcare coffin.
Whatever little public health infrastructure exists especially in rural and semi-urban areas, are far from good quality with very few exceptions and plagued by systemic inefficiencies, corruption, overloaded to a breaking point. The void in availability triggered the recent malpractices in C19 vaccine dissemination and testing, mushrooming of fly-by-night operators posing as healthcare providers for critical care in rural areas during the peak of the pandemic. These are just symptoms of the deep rootedness of the problem, arising out of lack of ethical governance, inefficiencies, and poor quality of our health infrastructure and its operating systems, with the lack of incentives and the knowledge to improve it systematically.

While the spending by India on public health has been relatively small compared to the scale needed, the demand for healthcare-related services has been growing steadily with increasing health awareness among a growing middle class comprising India’s large population of 1.38 billion. Out of this large population, almost 50% are the youth, who are less than 30 years of age. The size of the healthcare industry in India is currently about US$100 Bn and expected to accelerate and touch around US$ 135 to US$150 Bn by 2023, stimulated by the current health crisis ushered in by the C19 Pandemic.
The mismatch of the supply side, due to low government spending and growth of demand has resulted in a widening gap, that has motivated private sector players to invest in an unregulated manner. This sector is driven primarily by the profit motive, with a tendency for compromising the quality of patient care and safety in the name of efficiency enhancement, for reducing their operating costs. So, on one hand, we have the private system predominantly built on cost-driven quality with high efficiencies that may not always deliver value and quality care to patients. On the other side, we have a public health system, which is systemically inefficient resulting in higher intrinsic costs and of sub-standard quality. In both, cases the quality of healthcare is compromised. Though there are a few exceptions on both sides, they represent a minority.
Hence, this lack of quality, has resulted in an ecosystem of cost-based competition which does not focus on value maximization for the patient, and the ultimate payer of the services. This imbalance between public spending and private investment has also resulted in the development of an asymmetric industry structure with about 75% of health facilities represented by the private sector and 25% in the public domain. This ratio should actually be the reverse and at most equal given the context of a developing nation like India with stark economic inequalities, where the majority of the population are struggling below the poverty line, the rich-poor divide further aggravated by the C19 Pandemic. The poor and needy don’t have the wherewithal to pay for private healthcare and hence need health protection from a sound public system.
This private to a public ratio of 75:25 represents the structural problem and is the third nail in our healthcare coffin.
This distribution gets skewed further and links the geographical and the structural problem, through the above ratios. The majority of the private sector players have set up facilities for only serving the population in major metros cities and urban areas who represent the population with the spending power, without addressing the needs of semi-urban and rural areas who are having lower spending power, thus increasing the healthcare divide. This inequity is further reflected by the fact, that more than 80% of qualified doctors, nurses, and paramedics are employed by private hospitals. It leaves most public hospitals with resources stretched very thin, very few qualified doctors and nurses opting to serve in non-urban areas, hence most of the public hospitals in districts are understaffed by almost 70% from its sanctioned capacity, due to the unavailability of qualified healthcare professionals.
Therefore, even if the hard infrastructure is available in the districts the soft infrastructure of requisite quality is missing, making the public health system dysfunctional. The problem gets compounded while responding to crises such as that resulting from the C19 Pandemic. Therefore, the erroneous government policies have resulted in a dysfunctional industry and talent structure, where even the basic availability of healthcare services is a challenge for the vast majority of our population. This aberration in industry structure with dominant private sector interests has fuelled profiteering motives as seen in the current C19 Pandemic.
However, this is only the part and start of the problem, the future evolution of our healthcare services poses the greatest challenge as we seem to be on a collision course, with future Pandemic like health disasters, like we experienced recently. Whether we like it or not, such situations are going to be part of the turbulent environment, more likely to reoccur.
Unless we shift our thinking and deeply reflect on what track our healthcare should follow and how the change from the current track that leads to ‘doom’ be effected, we shall only end up hammering in, the final nail in our healthcare coffin.
Correction of the aberration in the industry structure due to lack of availability of public healthcare infrastructure resulting in the domination by private players in metro cities and urban areas, who are competing on costs rather than value creation, now needs to be brought on the value track founded on quality. The only way out is through a tectonic shift in thinking about a solution that flows from —a quality-driven value mindset. The incentive for the evolution of the healthcare industry on the quality track is of paramount importance as it deals with the criticality of impacting lives. The quality aspect has been unfortunately missing in most of the healthcare value chain, starting with our health policy design. Also, sustainable quality and affordable healthcare for all primarily arise from the capacity for value creation by all the actors of the ecosystem through consistent innovation rather than the unidimensional focus on cost, which has evaded the attention of our policymakers. Providing the right policy stimuli for transitioning the current cost-based system of our healthcare to a value-based competition, that evolves on the quality track to provide healthcare excellence at affordable costs to our citizens, should be the primary objective.
In any industry, competition should drive up value for customers as quality improves and costs fall. It is often argued that Healthcare is different from other sectors for this principle to be applicable as i)Healthcare delivery is complex ii)Customers are not informed iii) Services are highly customized. Healthcare undoubtedly has these characteristics, but so do other industries where competition works well. For example business of providing enterprise software or technical services to organizations is highly complex and customized, yet when adjusted for quality the cost of enterprise computing has fallen drastically over the last decade. Healthcare competition by contrast has become ‘zero sum’: system participants divide value instead of increasing it. In many cases, they create a ‘negative sum’ by adding administrative costs and pass it on to the payer or the patient in most cases.

Zero-Sum Competition Mindset in healthcare is manifested in several ways as follows:
Why the competition in our healthcare system is not focused on value, is the fundamental, unrecognized problem of our healthcare system. Competition is both too broad and too narrow. It is too broad as the competition occurs at the level of health plans, networks, hospital groups, physician groups, or clinics. It should occur in addressing a particular medical condition. It is too narrow as it occurs at the level of intervention or services and not over the full cycle like monitoring and prevention, diagnosis and treatment, and the ongoing management of the condition.
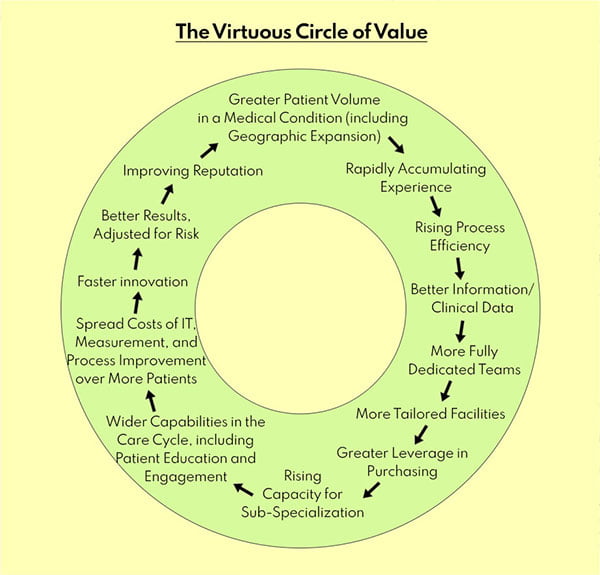
Value in healthcare is created or destroyed at the medical condition level and not at the level of hospital or physician practice. Information on what is most effective for a patient’s specific medical condition is non-existent or not furnished. What is furnished is what the hospital or network or physician provides, that is permitted by the health plan. Item 1 above, represents the virtuous cycle of value creation (Porter: HBR 2004) that leads to the higher quality of care, driving up efficiencies and lowering the overall cost of the treatment for the patient. This cycle in the Indian health system is truncated and hence does not evolve to benefit the patient, as well as the system as a whole, due to the wrong level of competition.
The right kind of competition on results at the level of medical conditions over the care cycle will lead to major improvements in inefficiency. It will also drive huge improvements in quality. But what is crucial to understand is that quality and cost will often improve simultaneously. The extent of this opportunity in healthcare is one of the most important and encouraging findings and it carries profound implications.
The widespread opportunity to achieve simultaneous improvements in cost and quality in healthcare arises for several reasons. First, much of healthcare delivery lacks the state of the art in best practices. This leaves ample room for simultaneous improvement in quality and cost, even in the short run. Just by implementing known best practices, virtually all providers can improve both quality and margins without raising prices.
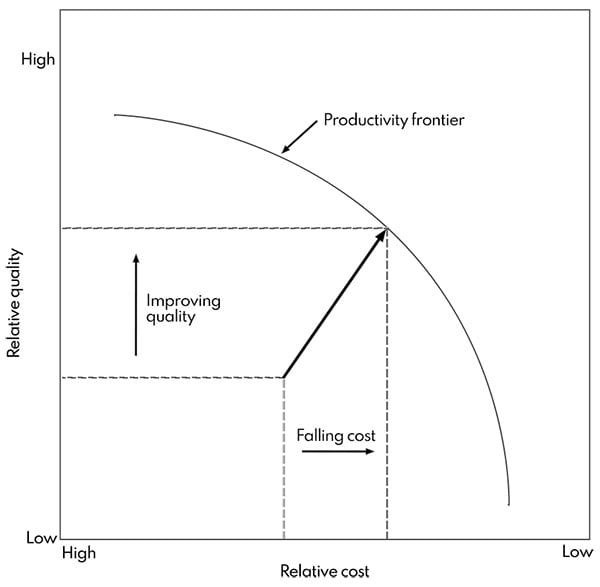
One may imagine a productivity frontier, which relates the quality of the health outcomes achieved in everything a particular medical condition to the full cost of providing care, for that condition, refer to Item 2. The productivity frontier incorporates all available best practices in terms of process protocols, technologies, drugs, and other aspects of care. If the provider is not at the productivity frontier, catching up and moving to the frontier will allow delivering current outcomes at lower costs, or improve outcomes at the same cost, or in many cases, attaining better outcomes at the lower cost. For example, timely administration of drugs will produce better results with no cost increase, or a new arthroscopic procedure may improve quality in terms of complications and recovery time while lowering costs through shorter operative time and time in hospital. When providers fail to use best practices, conversely, more spending will often not improve outcomes.
The policy or the lack of it that resulted in the proliferation of private healthcare players seeking to profit from the vacuum left by the public healthcare system resulted in the zero-sum competition, which has further triggered a revolutionary change in industry structure. Providers have rapidly consolidated, leaving behind only two or three vertically integrated networks consisting of hospitals and physician groups in many regions becoming quasi-monopolies, concentrating on providing quality healthcare to the relatively richer sections of the society in major Indian metro cities, who can afford to pay higher prices for treatment. These groups by virtue of quasi-monopoly status in their regions have developed bargaining leverage to escalate the prices of treatment.
The recent increases by private players have reset the prices of the managed care regime of the public system which has become weak due to the 75:25 structural aberration. It does not reflect an increase in any value but shifting the costs to health plans, employers and consumers, and the ultimate patients. The interplay of the factors of competition at the wrong level and the existing structural aberration triggered by wrong policies at the wrong time is a cycle that compounds the problem of availability and destroys any incentive for competition to evolve based on quality and innovation delivering value to patients who are the ultimate consumers of the healthcare system.
So far reforms have ignored the dynamics of competition and its impact on industry structure. Hence, the discussions on reforms should be driven by a deep understanding of the structure of healthcare delivery to patients and the crucial role of value-based competition, in driving improvements in quality, safety, and efficiency. Only competition on results to improve the diagnosis, treatment, management, and prevention of specific medical conditions, will lead to true value improvements for patients, in terms of both quality and cost.
Therefore, the reforms must focus on how to get competition right and how to put in place the enabling conditions to incentivize value creation through innovation and rooted in the principles of quality and safety, with the right information for patients, the right incentives for providers, the time horizons and the right mindsets for policymakers, promoters, and key stakeholders. All these ingredients have to be put together addressing resources, structure, talent, and competition to bring our healthcare on the value track and accelerate its journey towards excellence at par with the best in the world.
***